The Nebraska Biocontainment Unit was dedicated in 2005 and drilled for nine years to prepare for activation. The NBU is a collaborative project involving Nebraska Medicine and the University of Nebraska Medical Center. In addition to providing medical care for patients with highly hazardous communicable diseases, the unit has active research and outreach training programs for the region and nation. Unit personnel consists of a voluntary staff of select physicians, nursing, nursing assistants and respiratory therapists specially trained in high-level isolation and bio preparedness.
The NBU was activated in the fall of 2014 to receive U.S. citizens with Ebola virus disease medically evacuated from Africa. The outstanding staff received numerous awards for its courageous and extraordinary level of care including recognition from the White House, the Nebraska Legislature and the University of Nebraska Board of Regents. In addition, they were honored as "Midlanders of the Year" by the Omaha World-Herald. In 2020, the NBU was again activated for the care and management of U.S. citizens from Wuhan, China, and the Diamond Princess Cruise ship for COVID-19.
The Nebraska Biocontainment Unit was one of three units selected to care for United States citizens medically evacuated from Africa with the Ebola virus. The unit is a secured area with highly trained staff who safely provide all levels of care to patients infected with highly hazardous communicable diseases.
Some of the highly hazardous communicable diseases that the Biocontainment Unit may activate for include:
- Viral hemorrhagic fevers
- Ebola virus diseases (EVD)
- Marburg
- Lassa Fever
- Crimean Congo hemorrhagic fever
- Argentine hemorrhagic fever
- Bolivia hemorrhagic fever (Machupo)
- Respiratory pathogens
- Middle Eastern respiratory syndrome (MERS)
- Severe acute respiratory syndrome (SARS)
- Pneumonic plague
- Influenza like illness with pandemic potential
- Additional special pathogens
- Nipah virus infection
- Smallpox
- Mpox
- Disease X (Newly emerging special pathogens. These are diseases identified as highly communicable and hazardous)
Our staff
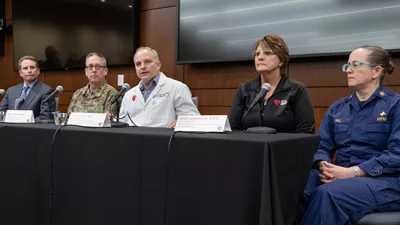
Headed by Medical Director Angela Hewlett, MD, an infectious diseases specialist, NBU personnel consists of an extraordinary staff of select physicians, registered nurses, respiratory therapists and patient care technicians specially trained in high level isolation and bio-preparedness. Most work full-time in other areas of Nebraska Medicine but remain on-call to report promptly for duty when the unit is activated.
The staff all receive specialized training and participate in numerous drills throughout the year. The entire unit is specially isolated from the rest of the hospital, using its own ventilation system and security access.
Download the Nebraska Medicine Biocontainment brochure
Unique features
Some of the unit's unique features include high-efficiency particulate air (HEPA) filtration system to ensure that micro-organisms do not spread beyond the patient rooms.
There is a secured access main entrance featuring double doors that are pressure controlled. Staff have a separate, secured access entrance and exit. Dual "pass-through" autoclaves decontaminate waste, linens, and materials leaving the unit.
Patient isolation rooms maintain negative air flow with 15 or more air exchanges per hour to assure that hazardous infections are contained.
Use of a secure telehealth communication system minimizes the number of staff needing to enter isolation rooms.
Use of HEPA-filtered individual isolation units, sometimes called biopods or isopods, are available for safe transport and transfer of an infected patient to the unit.
Media contact:
Taylor Wilson
- 402.871.8338 (cell)
- twilson@nebraskamed.com

In 2018, the United States Department of Health and Human Services awarded Nebraska Medicine/University of Nebraska Medical Center one of two national demonstration grants to address health care preparedness challenges, establish promising practices for improving disaster readiness across the health care delivery system, demonstrate the potential effectiveness of an RDHRS (Regional Disaster Health Response System), and make progress toward building a national system for readiness built on collaboration. The Region VII Disaster Health Response Ecosystem is directed by UNMC’s Global Center for Health Security leaders Shelly Schwedhelm and Dr. James Lawler, and recently launched a new website. For more information, visit Regionviidhre.com.