What is a pelvic organ prolapse, and how is it treated?
Pelvic organ prolapse is an uncomfortable condition that’s made worse by being a sensitive subject for people to talk about. Despite this difficulty, it’s important to know what pelvic organ prolapse is; as uncomfortable as it may be, it’s a treatable condition.
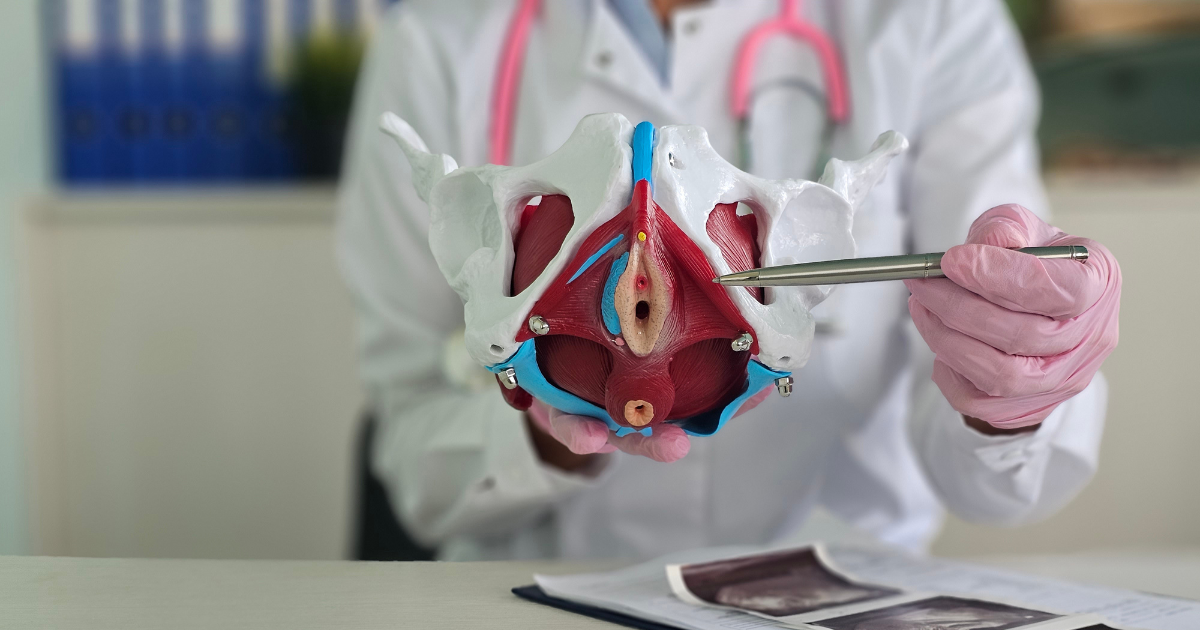
“Pelvic organ prolapse is a dropping of the pelvic organs – like the bowel, bladder or uterus – into the vaginal canal,” says urogynecologist and reconstructive pelvic surgeon Isuzu Meyer, MD. “You can think of the pelvic floor like a suspension, and when the suspension breaks, everything falls into the vaginal canal because it’s an open space.”
These organs moving can result in a visible bulge inside or outside the vagina. “It can be very uncomfortable but doesn’t typically cause pain,” says Dr. Meyer.
Types of pelvic organ prolapse
There are six primary types of pelvic organ prolapse:
- Dropped bladder (anterior vaginal wall prolapse)
- Enterocele (the small intestine bulging on the back or top of the vagina)
- Dropped rectum (posterior vaginal wall prolapse)
- Urethrocele (a droop or kink in the urethra)
- Dropped uterus (uterine prolapse)
- Vaginal vault prolapse (the top of the vagina falls after hysterectomy)
“The most common type of pelvic organ prolapse is a dropped bladder,” says Dr. Meyer. “Essentially, the vaginal wall and pelvic support that hold the bladder up fail, allowing it to drop into the vagina.”
Risk factors for pelvic organ prolapse
Some factors may increase your likelihood of a pelvic organ prolapse, such as:
- Pregnancy
- Multiple vaginal childbirths
- Pelvic trauma
- Repetitive heavy lifting – in an occupational setting
“A cesarean section should not be performed solely as a protective measure against pelvic organ prolapse,” says Dr. Meyer. “Still, a vaginal birth is considered a risk factor for the pelvic organs and support system.”
Symptoms of pelvic organ prolapse
Often pelvic organ prolapse has few symptoms outside a bulge inside or outside the vagina. “You could feel pressure inside the vagina,” says Dr. Meyer. “It can feel like you’re sitting on a golf ball or a similar object. This feeling can be very uncomfortable but doesn’t typically cause pain.
Diagnosing pelvic organ prolapse
Providers typically diagnose a pelvic organ prolapse through a pelvic examination. “The prolapse should be visible, and you don’t necessarily need any imaging or further tests,” says Dr. Meyer.
In special cases, a pelvic organ prolapse may require an MRI or other imaging for surgical planning. “Still, in most cases, we can diagnose it through a physical examination by itself,” says Dr. Meyer.
Treating pelvic organ prolapse
There are three primary treatments for pelvic organ prolapse:
- Expected management
- Pelvic floor exercises
- Vaginal insert
- Surgery
“The first option is to leave it alone and treat it through expected management,” says Dr. Meyer. If patients do not have any bothersome symptoms, they do not need any treatment.
Conservative treatments include pelvic exercises to ease your symptoms. Pelvic floor physical therapy is a great option, especially if patients have pelvic walls that haven't completely collapsed and desire to avoid further treatments.
“Additionally, if your pelvic walls are more collapsed, we can use a vaginal insert – like a pessary – to keep everything from dropping,” says Dr. Meyer. “We’re not fixing the problem, but it keeps your pelvic organs in place.”
The definitive treatment option for pelvic organ prolapse is surgery. If your pelvic walls have mostly collapsed, you can undergo surgery to “fix” the problem. Surgery for prolapse is relatively common. According to Dr. Meyer, 1 in 8 women will undergo surgical management for pelvic organ prolapse in their lifetime.
Deciding which treatment option is right for you depends on your particular symptoms. "It's a quality-of-life issue," says Dr. Meyer. "Pelvic organ prolapse isn't life-threatening; however, it significantly impacts patients' quality of life. I seek to support patients with shared decision-making to regain their lives.”
Providers base treatment decisions for a prolapse on a patient's symptoms. Consequently, each individual must choose treatment based on how uncomfortable their condition makes them feel and their goals.
“Ultimately, I can reconstruct the vagina and restore their anatomy, especially when pelvic organ prolapse is impacting other organs,” says Dr. Meyer. “In instances where a prolapse is affecting pelvic organs like the bladder or rectum functions, I often recommend treating a pelvic organ prolapse surgically.”
Preventing pelvic organ prolapse
Although research is still ongoing, there is little data on preventing pelvic organ prolapse. “While physical therapy won’t repair the prolapse, it will strengthen the existing pelvic floor support to ensure the condition doesn’t worsen,” says Dr. Meyer.
“Occasionally, this physical therapy can even lead to some improvement by fortifying the surrounding structures.” In addition to physical therapy, losing weight can decrease your risk of pelvic organ prolapse if you are obese.
Living with pelvic organ prolapse
“Pelvic organ prolapse is not a normal part of aging, and we're here to help," says Dr. Meyer. "Existing research demonstrates that these women suffer in silence for a long time. It often takes several years from when patients become symptomatic to when they seek care.”
However, seeking treatment for pelvic organ prolapse is critical to improving their quality of life. "There are many things we can do to help," says Dr. Meyer.







