Swallowing surgery gives patient his life back

It all happened so quickly.
One day, Gary Gonzales sat around the dining room table laughing and enjoying Christmas dinner with his family. The next day, Gary couldn’t get a bite of food down.
Every time Gary tried to eat, the food would make its way down his throat and then seemed to get lodged in his lower esophagus, eventually coming back up. It was painful and uncomfortable. These strange symptoms continued for days with no relief. It became so bad that Gary became fearful of eating.
So Gary, then 74, made an appointment to see his family doctor, who referred him to Nebraska Medicine gastroenterologist Kathryn Hutchins, MD.
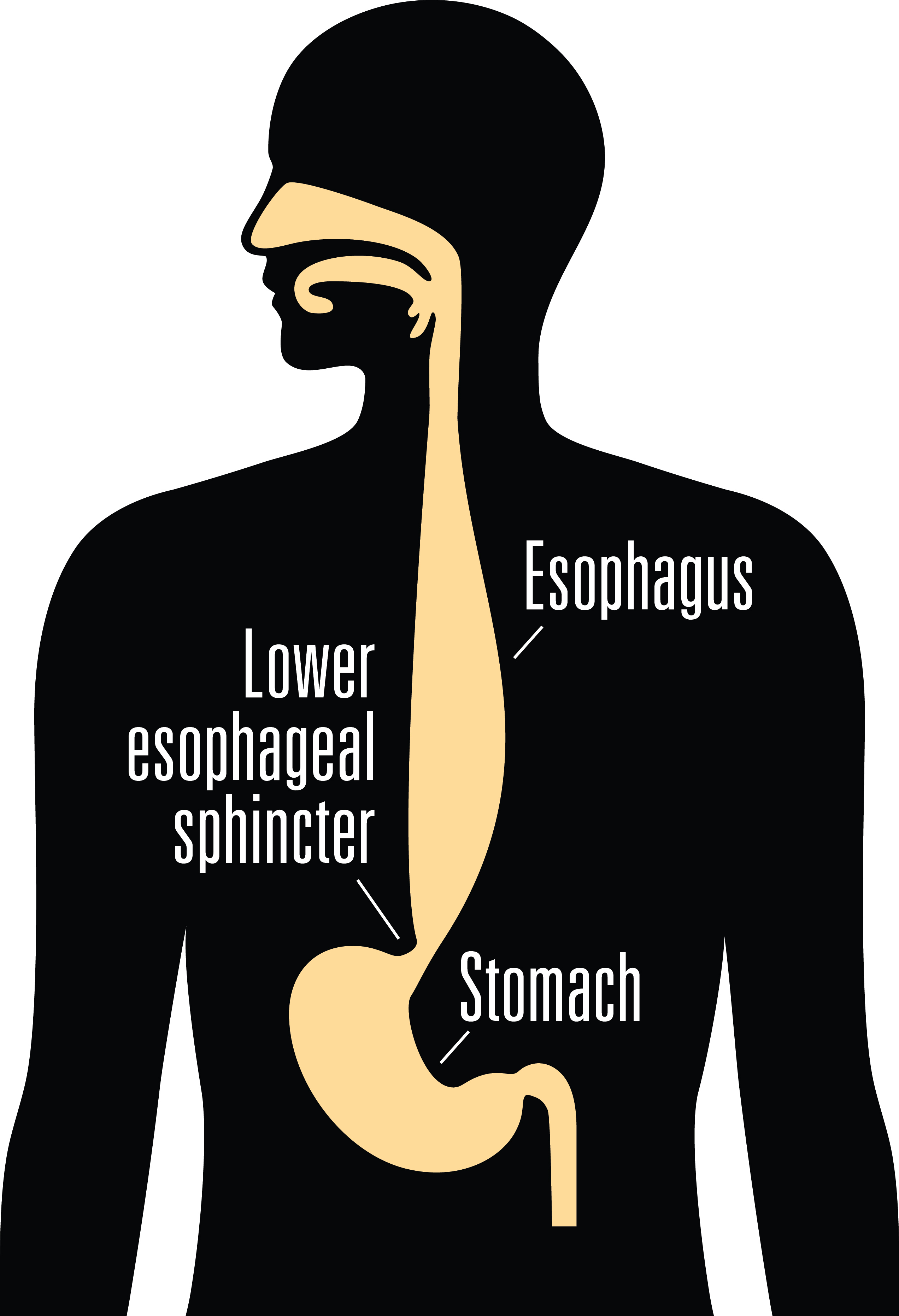
Several tests later, Gary was diagnosed with esophageal achalasia, a rare disorder that makes it difficult to swallow. It occurs when the nerves in the esophagus (the tube that carries food from your throat to your stomach) are damaged, preventing the esophagus from functioning properly. As a result, food travels more slowly down your esophagus, and the muscles in the lower esophageal sphincter (the valve between the esophagus and the stomach) fail to relax properly, preventing food from entering the stomach. This results in difficulty swallowing, regurgitation of food, chest pain and sometimes weight loss.
Shortly thereafter, Gary was scheduled to have a Heller myotomy surgery. Heller myotomy is a minimally invasive procedure that cuts the lower esophageal sphincter muscle to allow food and liquids to pass into the stomach. A fundoplication is often performed at the same time, which helps reduce the risk of acid reflux after surgery. After his surgery, Gary says he was immediately better.
But the relief only lasted a few months before the symptoms began to return.
This time, the symptoms grew worse. While Gary would usually manage to get down some food at meals, he would experience severe regurgitation at night. “The food would make its way back up the esophagus while I was sleeping,” explains Gary. “I would wake and felt like I was strangling. I would cough and cough and often end up throwing it all up.” Sometimes, the regurgitation would repeat itself as soon as Gary fell asleep again.
 Gary also experienced incidents in which the food became lodged in his esophagus, preventing him from eating or drinking. During two of these incidents, he had to go to the emergency room. A tube had to be threaded down his throat and was used to push the food through until it became dislodged.
Gary also experienced incidents in which the food became lodged in his esophagus, preventing him from eating or drinking. During two of these incidents, he had to go to the emergency room. A tube had to be threaded down his throat and was used to push the food through until it became dislodged.
The regurgitation episodes also caused Gary to develop pneumonia several times due to food aspirating into the lungs. Twice, these episodes required hospitalization. Gary struggled with these unpleasant symptoms for more than five years until he finally connected with Nebraska Medicine gastroenterologist Alexander Hewlett, MD, who worked closely with Gary to try to relieve his symptoms. Dr. Hewlett prescribed several medications, but none helped.
Dr. Hewlett knew that if Gary’s condition continued, the consequences could be fatal. Dr. Hewlett referred Gary to Ivy Haskins, MD, Nebraska Medicine minimally invasive general surgeon. The two are part of a multidisciplinary group of doctors and health care professionals who treat and manage all types of esophageal and gastrointestinal disorders, including swallowing disorders, reflux, hiatal hernias (hernias that occur in the diaphragm) and stomach emptying problems.
After additional scans, Dr. Haskins discovered that a pouch (diverticulum) had formed in the esophagus wall that was trapping food and liquids. Dr. Haskins recommended surgery to remove the diverticulum and revision of his previous Heller myotomy surgery.
“Patients with this type of condition risk failure to thrive due to their inability to keep food down,” says Dr. Haskins, who performs 20 to 30 of these surgeries a year. “Gary was also considered a high-risk patient because of his recurrent episodes of aspiration pneumonia and previous Heller myotomy.”
In September 2023, Gary underwent a second Heller myotomy procedure, this time with resection of the diverticulum. Dr. Haskins also performed a fundoplication procedure in which the top part of the stomach is wrapped around the lower esophageal sphincter to reinforce it and prevent reflux.
“Gary has had nearly full relief of symptoms,” says Dr. Haskins. “Our multidisciplinary approach to these types of disorders really contributes to the successful and expedient care of these patients. They are often discussed at our bi-monthly conferences to develop timely care plans and ensure the patient has been scheduled for surgery within one month of diagnosis. We realize the seriousness of this condition and the risk for failure to thrive it poses to patients.”
“My life has been infinitely better since the surgery,” says Gary. “I am better now than I have been for years. I feel like I got the best care a person could get. Dr. Hewlett, Dr. Haskins and the rest of the staff were genuinely concerned and did everything they could to help me.”
Gary is 80 years old now, and he and his wife, Julie, are finally getting back to enjoying life again without the constant worry and embarrassment of swallowing problems or reflux while out with friends and family. “The way I look at it, Dr. Haskins not only saved my life, but she has given me my life back,” Gary says.
Call 800.922.0000 to schedule an appointment with one of our swallowing disorder experts.





