Migraine remedies and when to see a doctor

More than 12% of the U.S. adult population suffers from the condition known as migraine. While women, men and children may experience migraine headaches, among adults, they are about three times as common in women.
Unfortunately, there is no cure for migraine. However, according to neurologist and headache specialist Peter Soh, MD, MPH, there are a range of options to treat and prevent migraine headaches.
“It’s a chronic condition, however, it’s highly treatable,” Dr. Soh says. “Treatments can be very helpful and reduce symptoms not just of the headache pain, but other bothersome associated symptoms.”
While medication is often used to treat migraine, there are also simple steps that can be taken to cope with the condition. The following “remedies” include lifestyle, behavioral and medicinal therapies.
Environmental changes
- Adjust the lighting, noise level. Migraine sufferers may be photophobic, or light sensitive, and/or phonophobic, or sound sensitive. Migraine sufferers may also have sensitivity to strong or specific odors.
Behavioral modification
- Reduce stress. Managing stress is important since stress can trigger migraine headaches
- Improve sleep. Sleep disruption or sleeping too much or too little may trigger migraine, so it is important to practice good sleep hygiene
- Eat well. Skipping or delaying meals can trigger migraine headaches. Alcohol, chocolate, aged cheeses, MSG, artificial sweeteners, caffeine, nuts, nitrates, artificial red food coloring (red no. 40), and citrus fruits can be a trigger for migraine headache
Self-monitoring
Keeping a headache diary or journal can be a powerful tool for patients. Not only does it gather valuable data for providers, but it helps patients understand their patterns and potential triggers. A daily diary can reveal what is working well and what may be making things worse.
“It’s a very simple, costless way for patients to track their headache frequency and severity, the medications they are taking, and the responsiveness of those headaches,” Dr. Soh says.
It may also be helpful to track any noticeable triggers for headaches in the diary, as well as cycle information for menstruating women.
Medications
Some patients will require medication to manage migraine. Acute treatment stops a migraine headache as early as possible, while other medications are taken to prevent them.
- Beta-blockers. Medications that lower blood pressure may also help prevent migraine headaches
- Antidepressants. Certain tricyclic antidepressants may help prevent migraine headaches
- Anti-seizure medications. Even if a patient does not have seizures, anticonvulsant medications may help prevent migraine headaches
- CGRP (calcitonin gene-related peptide) monoclonal antibodies. First preventive medicines specifically developed for the prevention of migraine. These are given by subcutaneous injection or IV infusion either monthly or quarterly depending on the medication
- Gepants. These are amongst the newest treatments for migraine and provide preventive and acute treatment. They belong to a class of medications known as CGRP receptor antagonists and are given orally
- Ditans. Another newer option for the acute treatment of migraine, ditans do not have vasoconstrictive effects. Therefore, they may be safer than the triptans for patients who have had heart attack, stroke, or have high blood-pressure
- Triptans. These are used once headache pain has begun. Due to their vasoconstrictive effects, they may not be suitable for patients who have a history of stroke, heart attack, or have high blood-pressure
Advanced intervention procedures
- Nerve blocks. A nerve-numbing medication is injected into the area around a nerve to reduce or stop the pain of an acute migraine attack
- Trigger point injections. These may reduce pain associated with areas of taut muscle fibers around the head and neck
- Botox® injections. Initially developed to reduce wrinkles, these have become a safe and effective treatment for chronic migraine
- Outpatient infusion therapy. Medication is administered intravenously to provide faster and potentially more effective pain relief for migraine pain
Nonpharmacological approaches
- Noninvasive neuromodulation by stimulating the nervous system through the skin with an electric current
- Vitamins, such as vitamin B2 or riboflavin, magnesium and CoQ10
- Biofeedback, cognitive behavioral therapy and relaxation training
- Physical therapy
- Acupuncture
- Massage therapy
When should I see a doctor?
When patients have disabling headaches that affect the quality of their life, they should see a provider. However, pain does not need to be disabling to warrant evaluation and treatment.
“Even if a patient is having moderate pain and the intensity of their headaches is not keeping them from their activities, they should see their doctor,” Dr. Soh says.
Headache specialists at the Nebraska Medicine Pain Clinic perform a thorough review of a patient’s history and a physical exam. During evaluation, specialists:
- Look for secondary causes or red flags that require further diagnostic testing
- Consider other contributing factors once secondary causes have been ruled out, such as low vitamin B12 or thyroid hormone
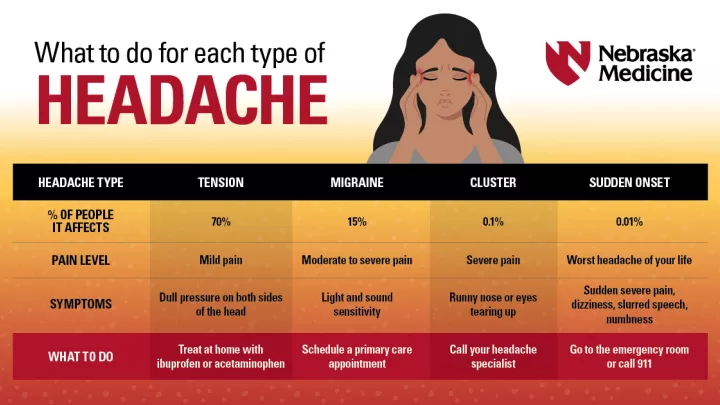
- Evaluate the patient’s symptoms to determine what type of headache disorder they may have
A multidisciplinary approach allows the team to tailor treatment to each patient’s unique needs and preferences. Dr. Soh says the team is dedicated to both relieving pain and preventing future attacks.
“Our therapeutic goal as headache specialists is to prevent recurrent headaches and, if a headache does break through, provide a rescue therapy that can be taken safely and effectively so patients can return to their normal lives.”