How the HPV vaccine could cure cervical cancer

The most common sexually transmitted infection in the United States, the human papillomavirus will infect a high percentage of sexually active adults at some point in their lives. While HPV often disappears on its own, for some it may lead to genital warts or cancers of the vulva, cervix, vagina, anus, penis, or oropharynx. Unfortunately, there isn't a way to know who will develop an HPV-related health problem.
According to the Centers for Disease Control and Prevention, nearly all cervical cancer cases are linked to HPV, affecting nearly half a million women worldwide every year. Once the leading cause of cancer death among women in the U.S., it is now one of the most preventable, thanks to the HPV vaccine and cervical cancer screenings.
Vaccination in early adolescence reduces cervical cancer risk
The ideal timeframe for HPV vaccination is age 11 to 12 years, while a pre-teen's immune response is at its best and before potential exposure to the HPV virus. Still, there is a vaccination hesitancy in the U.S., and the HPV vaccination rates are lagging behind other routine vaccines.
"There is stigma around HPV because it is thought of as a sexually transmitted infection," says Andreea Newtson, MD, Nebraska Medicine gynecologic oncologist. "While HPV is sexually transmitted, the CDC estimates that nearly every sexually active adult will be exposed to HPV in their lifetime. Infection is inevitable. We need to think of HPV less as an STI and more like the common cold. The stigma is preventing people from getting one of the only vaccines we have that can actually prevent cancer."
A study in the United Kingdom showed an 87% reduction in cervical cancer rates when vaccinated between ages 12 and 13. The reduction rate decreased with increasing the age of vaccination, supporting vaccination earlier in adolescence.
Dr. Newston says 90.1% of adolescents were vaccinated against Tdap in 2020, but only 58.6% were up-to-date on their HPV vaccine.
"I can't imagine that teens are more afraid of tetanus than of genital malignancies and genital warts," Dr. Newston says. "The way we think about HPV needs to change."
The HPV vaccine and the possibility of eliminating cervical cancer
The latest HPV vaccine (Gardasil 9) protects from nine common types of HPV found in 90% of cervical cancers.
"Statistical modeling from the World Health Organization estimates that, under certain conditions, cervical cancer has the potential to be nearly eradicated by 2120," says Dr. Newston. "At this moment, we have the tools to do this."
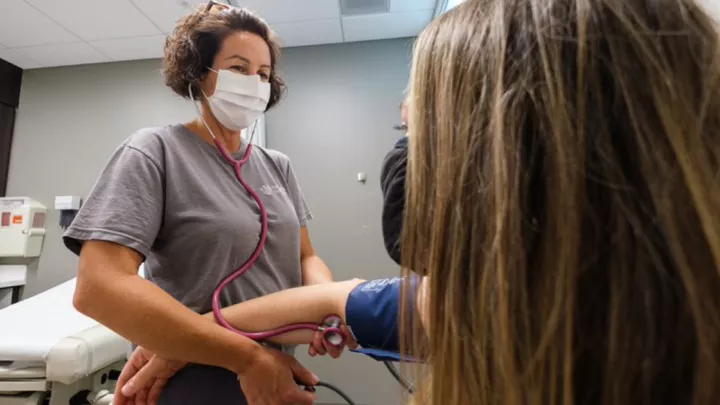
Even with vaccination, regular preventive screening is necessary
Although HPV vaccination dramatically decreases the risk of cervical cancer, it doesn't negate the need for screening.
"The HPV vaccine will give your immune system a major advantage in fighting off the virus before it can cause cancer, but it's not perfect," says Dr. Newston. "That's why it's still important to get your PAP smears and pelvic exams."
What about HPV vaccination after age 26?
"The vaccine is most effective if given before HPV exposure," says Dr. Newston. "That is why it is is so important to get our children vaccinated, because HPV is inevitable, just like catching a cold. But it is still highly effective if given after exposure."
However, Dr. Newston says with age, the strength of the immune system wanes and the risk of exposure increases, so vaccine efficacy decreases.
"If you get vaccinated later in life, staying on track with your PAP smears will be even more important. Those screenings help us catch cervical dysplasia and cervical cancer early," says Dr. Newston. "If you are worried about being too old to get the HPV vaccine, it will be OK. The PAP smear is still a very powerful tool in the prevention and early detection of cervical cancer."
If you've put off screenings or vaccinations, it's time to get back on track
Many people have delayed screenings and preventive doctor visits due to COVID-19. While understandable, cervical precancer and cancer are easier to treat when caught in the early stages.
The recommendation is for those ages 9 to 14 to receive two vaccine doses. Those older than 15 or those immunocompromised (ages 9 to 26) should receive three doses over 6 months.
"The rate of stage 4 cervical cancer is rising," says Dr. Newston. "We have had the tools to eradicate this type for cancer for decades, so this statistic is devastating. These deaths are completely preventable. Please get yourself and your loved ones vaccinated today. And if it's been a while since your last PAP smear, don't worry about that. Just make the appointment and come see us. A little late is better than not at all."
To make an appointment, contact your Primary Care doctor or OB-GYN.
If you do not have a Primary Care doctor, you can schedule an appointment with one online, or call 800.922.0000 to make a new patient appointment.
If you'd rather see an OB-GYN, you can browse a list of our OB-GYNs here and call their clinic to get something scheduled.