Using deep brain stimulation to treat movement disorders
Movement disorders are a category of neurological conditions that cause atypical movements. Common movement disorders include:
- Essential tremor – can run in families and results in head, face, hands or leg tremors.
- Parkinson’s disease – a brain disorder resulting from the loss of brain cells that secrete dopamine, a chemical that is necessary for normal movement. This results in tremors, slow movement and rigidity in arms and legs.
- Dystonia – concurrent activation of two opposing muscle groups resulting in abnormal, and often repetitive, movements or postures.
- Ataxia – a group of disorders that affect coordination, balance and speech, resulting in awkward or clumsy movements and changes to speech.
There are two major types of tremors that those with movement disorders experience: resting and intention tremors. Resting tremors – like those common in patients with Parkinson’s disease – occur when your body is relaxed, such as when watching TV. Intention tremors – like those common in patients with essential tremors – occur with voluntary muscle contraction, such as your hand shaking when reaching to put your key into the door.
Deep brain stimulation for movement disorders
“You can think of the deep brain structures – including the basal ganglia and thalamus –as a radio tower sending out signals for proper communication,” says neurosurgeon Aviva Abosch, MD, PhD. “When these structures function normally, the brain tells your motor cortex to move, and the resulting movement is normal.”
“However, when the signal emitted from these deep brain structures is abnormal, the movement becomes abnormal too. So, the radio tower is still transmitting, but the information is incorrect and leads to motor symptoms such as tremor, rigidity or slowed movements – called bradykinesia.”
Fortunately, if you impose a more typical pattern on the information being emitted from these brain structures, you can decrease or even eliminate the abnormal information and allow normal movement to take over again. Deep brain stimulation, or DBS, can re-establish these more typical brain signals.
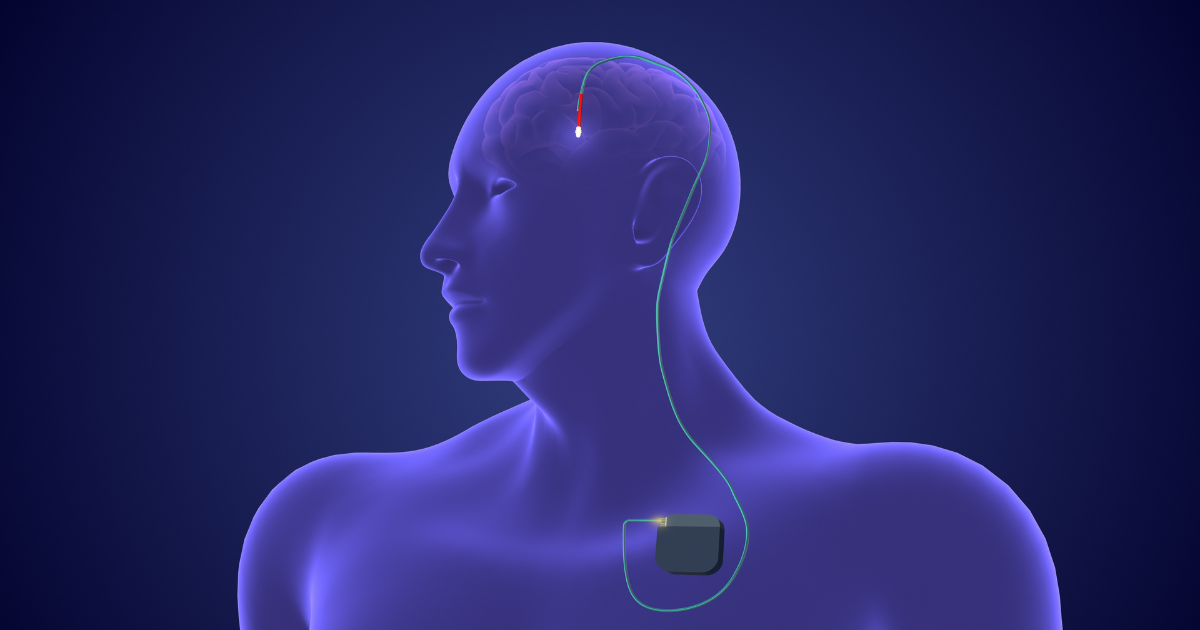
“Deep brain stimulation involves implanting a lead into a precise location in one of these deep brain structures, approximately 9 cm from the surface of the brain, and connecting this lead to an implantable pulse generator, or IPG, underneath the skin of the chest,” says Dr. Abosch.
The lead receives information that the movement disorder neurologist programs into the implantable pulse generator. Your physician can program the IPG externally with a computer wand to tell the device how to stimulate – i.e., which of the lead’s four contacts to use for emitting electrical stimulation, the frequency of the stimulation, its amplitude, and pulse width.
“These different parameters create a parameter space that your physician can fine-tune to your specific symptoms, so you receive the best efficacy from stimulation, meaning the optimal treatment of your symptoms,” says Dr. Abosch. Your physician will base this programming on the deep brain target selected by your physician, your unique brain features, your specific condition and your individual symptoms.
Who’s a candidate for deep brain stimulation?
“There’s a pretty involved process of working patients up for deep brain stimulation surgery,” says Dr. Abosch. “Ensuring that we are selecting the appropriate patients and therapy requires an extensive preoperative evaluation.”
“First, patients must fail standard medical therapy – medications for the specific movement disorder – at reasonable doses, pushed to the point of side effects,” says Dr. Abosch. “We also administer formal neuropsychological testing to determine what cognitive domains are, or are not, affected.”
Anyone who has even early signs of dementia on these formal neuropsychological tests isn’t a candidate for DBS surgery. “The reason to exclude patients with even early signs of dementia is that this procedure can expedite cognitive decline if already present,” says Dr. Abosch.
This neuropsychological testing also includes depression screening – as approximately 30% of the Parkinson’s population also has depression. “We want to determine if there’s untreated depression so that we can address it before surgery,” says Dr. Abosch.
Potential candidates for DBS surgery will also undergo clinical imaging in the form of an MRI. This imaging can rule out any other conditions that might progress over time, such as brain tumors or strokes.
“We also use formal rating scales to assess somebody’s tremor or their Parkinson’s motor symptoms – which include tremors, resistance to movement and slowness of movement,” says Dr. Abosch. “This assessment helps us when talking to patients about what benefits to expect from surgery.”
Finally, the Nebraska Medicine Multidisciplinary Movement Disorders Conference meets to discuss patients and decide who is or isn’t a candidate for deep brain stimulation surgery. This group reviews all of a patient’s clinical data and determines who’s a good candidate, who needs to be optimized clinically first, and who isn’t a candidate for DBS surgery.
Post-operative care for DBS surgery
Deep brain stimulation surgery for movement disorders typically requires an overnight stay in the hospital, although patients generally leave the next day. “Managing blood pressure is crucial, especially in the operating room,” says Dr. Abosch. “High blood pressure can result in bleeding in a critical brain area during surgery.”
You’ll also receive instructions on how to care for your surgical incisions in the immediate future. Likewise, you’ll need to avoid lifting anything heavy after surgery – as it can increase the pressure inside your head and cause problems with healing.
Because these devices are implanted for life, you must also be wary of infection. “If a patient with an implanted device gets bacterial pneumonia or has a cut they don’t treat promptly, for example, bacteria can enter the patient’s bloodstream and contaminate any implanted device,” says Dr. Abosch.
“Once bacteria contaminate your device, the device typically must be removed because you can’t clear an infection on an implanted device due to the absence of a blood supply to the device,” says Dr. Abosch. “So, antibiotics, even if given by IV, won’t clear the infection. Consequently, you’ll need to evaluate and treat any infections promptly and take antibiotics before going to the dentist for teeth cleaning,” says Dr. Abosch. “It’s no different than someone with a cardiac pacemaker, prosthetic valve or hip replacement.”
Living with a movement disorder
While not necessarily uncommon, movement disorders are NOT well-known enough for most people to understand them. “People can see a tremor and misunderstand what that person is going through,” says Dr. Abosch. “Not everyone has familiarity with these conditions, and some patients have complained to me that people have accused them of being drunk when it’s just their movement disorder tremor.”
“Because people generally have more understanding of conditions for which there is greater awareness, such misunderstanding can be quite detrimental and even impact patient employment status,” says Dr. Abosch.







