Aortic dissection symptoms, diagnosis and treatment
Aortic dissection is a serious, potentially life-threatening condition that can occur at any age. Knowing what the aorta is and what it does helps better understand the condition.
The aorta and what happens when a dissection occurs
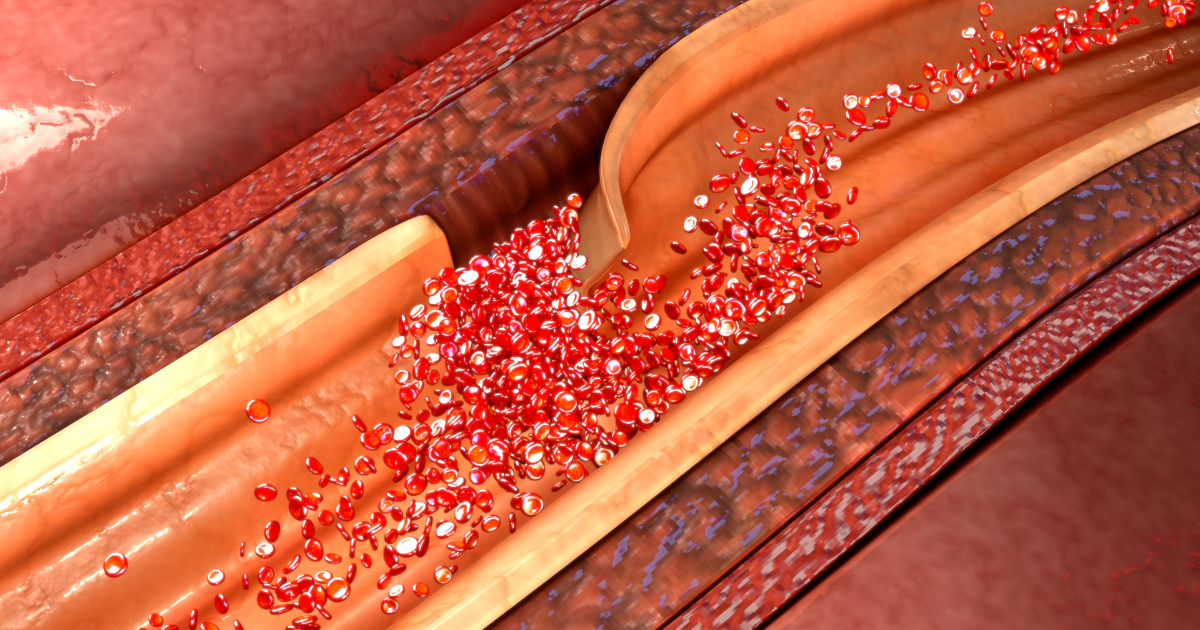
The aorta is the body’s largest artery that carries oxygen-rich blood, nutrients and hormones away from your heart to the rest of the body. It’s a long, tubular blood vessel that starts in the heart's left ventricle and travels upwards toward the head. It then curves from the front to the back of the chest, supplying the arms, head, chest and abdomen before finally dividing to supply the legs.
“The aortic wall has three layers,” explains thoracic and cardiac surgeon Aleem Siddique, MBBS. “With an aortic dissection, the inner wall of the tubing tears in a weakened area of the aorta and causes blood to surge through the layers of the wall.”
As blood flows between or through the tissue layers, blood flow to body parts and organs can be slowed or stopped, with the risk of the aorta rupturing completely.
“Since the aorta is a long blood vessel, the entire length may not tear,” adds Dr. Siddique. “Where it tears impacts the seriousness of the problem, and the symptoms vary depending on where the tear is located. This differentiation is important for how we assess the severity of the issue and how we manage it.”
Aortic dissections are divided into two main types:
- Type A involves the ascending aorta: The first part of the aorta is in the front of the chest and closest to the heart. This type is more common and more dangerous. The impact of the tear can be localized or spread along the entire length of the aorta.
- Type B involves the descending aorta: The part in the back of the chest that runs into the abdomen further from the heart.
Symptoms and risk factors
Typically, people with aortic dissection suffer sudden severe chest pain that may or may not spread to the upper back. “Usually people know right away that something isn’t right, feeling that something dramatically wrong has happened,” adds Dr. Siddique. “Although sudden chest pain is common, not everybody experiences it. Some people present with other complaints related to the tear's effect on other blood vessels and organs, which may look like stroke-like symptoms.”
Symptoms that warrant immediate emergency care include:
- Sudden severe, sharp chest pain with or without upper back pain. This kind of pain doesn’t come and go. People may describe a tearing or ripping sensation.
- Abdominal pain.
- Shortness of breath.
- Low blood pressure, fainting, dizziness or confusion.
- Stroke-like symptoms, including weakness or numbness on one side of the body or trouble talking.
Aortic dissection can cause additional issues like hypertension, stroke, accumulation of fluid suddenly around the heart or lungs (effusions), kidney problems, or a cold, numb or painful limb.
Why do aortic dissections happen?
“There seems to be a structural reason why a person might be vulnerable to an aortic tear,” says Dr. Siddique. “Some may be predisposed to aortic dissection caused by an inherited gene compounded by other health factors.”
See how the Nebraska Medicine Genetics Clinic helps patients get control of complex heart conditions.
Risk factors include:
- Family history of aortic dissection. If you have someone in your family who has had an aortic dissection, relatives should be screened to ensure they are not at risk.
- Pregnancy with high blood pressure during delivery.
- Uncontrolled high blood pressure.
- A buildup of plaque in the arteries (atherosclerosis).
- High cholesterol and smoking.
- Heart conditions you were born with, including bicuspid aortic valves or Turner syndrome.
- Aortic aneurysm, aortic valve disease or genetic connective tissue disorders like Marfan syndrome or Ehlers-Danlos syndrome.
- Traumatic injury to the chest.
Diagnosis and treatment
Often, an aortic dissection occurs suddenly, requiring immediate medical intervention. In the emergency room, your healthcare team will do tests to rule out a heart attack or stroke (which can present similar symptoms). A CT scan is necessary to make a diagnosis.
A person may only discover they have the condition incidentally, as it may be found during a CT scan for another reason.
Treatment depends upon the location of the tear and dissection
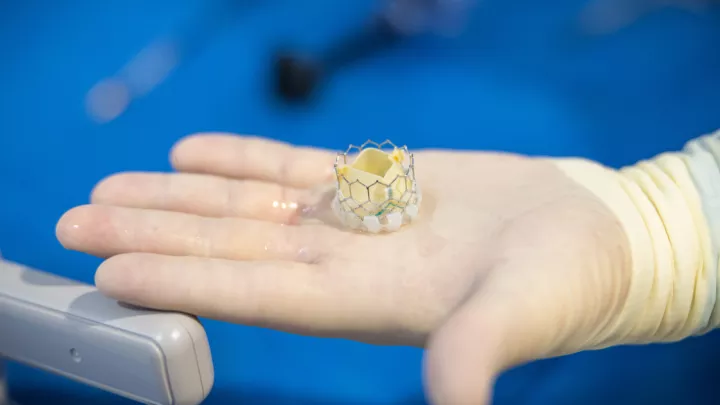
Type A dissection requires immediate, complex surgery to remove and replace the part of the blood vessel that is torn, as the most life-threatening part is closest to the heart. When promptly treated, surgery offers an 80 to 90% survival rate. While surgery can significantly improve survival chances, risks and potential long-term impacts remain. Long-term follow-up is necessary, including regular CT scans.
Type B dissection may need surgery urgently if the tear cuts off the blood flow to vital organs. However, other organs are more commonly not involved, so this type is usually managed conservatively initially.
“When dealing with Type B, we manage the pain, control the blood pressure, and monitor them closely,” says Dr. Siddique. “In the long term, many patients' aorta changes over time; in particular, it may become enlarged – aneurysmal. A third of patients require surgery in the long term due to these changes. Some patients may benefit from pre-emptive early surgery in cases where the dissection has concerning features for future enlargement. Therefore, patients must be followed long term with regular CT scans, especially in the first five years after the dissection.”
Preventive measures focus on factors that can be changed, such as controlling blood pressure, avoiding smoking and practicing a healthy lifestyle.
See how a thoracic branch graft procedure improves outcomes for patients with aortic tears.